Introduction to Range of Motion (ROM) in Healthcare
Range of motion (ROM) is a foundational concept in physical and occupational therapy. It refers to the extent of movement that a joint can achieve in various directions. For therapists, understanding and optimizing ROM is critical for patient recovery and overall well-being. This post dives deep into the different types of ROM, its importance, and practical tips for incorporating ROM exercises into therapy sessions.
Understanding Passive Range of Motion (PROM)
Passive Range of Motion (PROM) involves movement applied to a joint by an external force, such as a therapist’s hands, without any effort from the patient. PROM is essential for patients unable to move a joint independently, often due to injury, surgery, or neurological conditions.
Role of PROM in Therapy
PROM helps maintain joint flexibility, improve circulation, and prevent joint stiffness. By moving the joint through its available range, therapists can keep tissues pliable and promote healing. PROM exercises are particularly crucial in the early stages of rehabilitation when active movement might be limited.
Examples of PROM Exercises
- Wrist Circles: The therapist gently rotates the patient’s wrists in circular motions.
- Shoulder Flexion: The therapist moves the patient’s arm upward and over the head while the patient remains relaxed.
- Bicep flexion and extension: The therapist guides the patient’s elbow away from and towards the midline of the body.
Incorporating these exercises ensures that patients retain some joint flexibility, even when they cannot actively participate.
Exploring Active Range of Motion (AROM)
Active Range of Motion (AROM) refers to movements performed entirely by the patient without external assistance. AROM is integral to strengthening muscles, enhancing coordination, and promoting independence in daily activities.
Significance of AROM in Rehabilitation
AROM exercises help patients build muscle strength around the joint, improve motor control, and regain functional abilities. These activities encourage patients to take an active role in their recovery, which can boost motivation and adherence to therapy programs.
Examples of AROM Activities
- Wrist Flexion and Extension: The patient bends the wrist forward and backward.

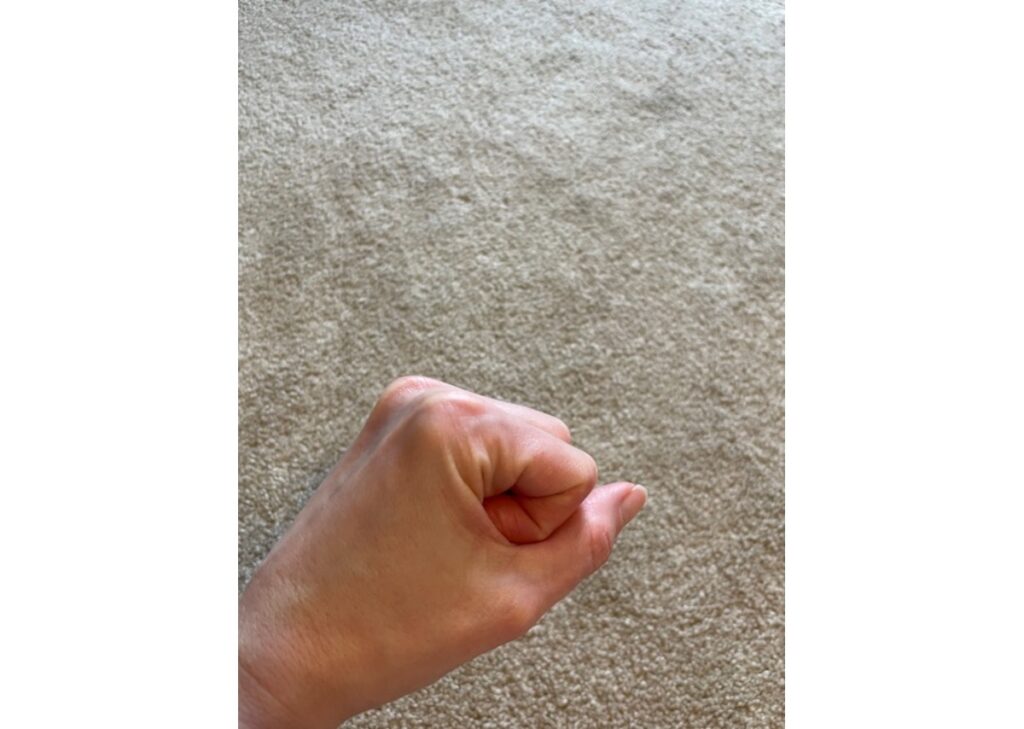
- Digit Flexion and Extension: The patient straightens and bends the fingers.
- Thumb Abduction: The patient moves the thumb away from the digits.

By incorporating AROM exercises, therapists can tailor interventions to individual patient needs, promoting optimal recovery outcomes.
Understanding Active Assisted Range of Motion (AAROM)
Active Assisted Range of Motion (AROM) refers to movements performed by the patient with external assistance. AAROM is integral to strengthening muscles, enhancing coordination, and promoting independence in daily activities.
AAROM Exercises for Shoulder and Wrist Rehabilitation
Assisted Active Range of Motion exercises play a crucial role in helping patients incrementally regain their active range of motion (AROM). For instance, if a patient can achieve AROM to 60 degrees of shoulder flexion independently, a therapist or trained caregiver can assist the patient to reach 90, 120, or even 180 degrees. In situations where patients need additional support, objects such as towels can help bridge the range gap.
Shoulder Flexion Example:
A patient may have full range of motion of 180 degrees in the right shoulder while experiencing a decrease in AROM due to a rotator cuff injury on the left shoulder. After receiving clearance from the doctor, the patient is guided to begin ROM exercises aimed at restoring full motion. Following the therapist’s instructions, the patient uses a towel for assistance.
- The patient grasps the ends of the towel with both hands, ensuring arms are extended while lying supine on the bed.
- The patient is instructed to slowly lift the arms over the body towards the head, maintaining a straight position as tolerated without pain.
Wrist Deviation Example:

Another effective example of AAROM can be used for wrist movements, specifically ulnar and radial deviation. In this exercise:
- The patient sits in a chair positioned in front of a table with a dry washcloth placed under the hand.
- The patient then rotates the wrist to the left and right, mimicking the movement of a windshield wiper, to gradually increase their range of motion.
Regularly incorporating these exercises into therapy can significantly assist patients in their rehabilitation journey, enhancing their independence and overall functionality.
The Difference Between a Joint’s Possible Range of Motion and Its Actual Range of Motion
A joint’s possible range of motion refers to the maximum movement it could achieve under ideal conditions, considering anatomical structures. In contrast, the actual range of motion is the movement a joint can achieve in real-life scenarios, often limited by pain, stiffness, or muscle weakness.
Factors Affecting ROM
Several factors influence both possible and actual ROM, including:
- Age: Younger individuals generally have greater flexibility than older adults.
- Injury: Trauma or damage to joints can reduce ROM.
- Muscle Strength: Weak muscles can limit the ability to move a joint through its full range.
Understanding these factors allows therapists to develop targeted strategies for improving ROM.
Measuring and Improving ROM
Therapists use tools like goniometers and inclinometers to measure joint angles and assess ROM. Regular assessments help track progress and adjust treatment plans accordingly. Techniques like stretching, strengthening exercises, and manual therapy can enhance actual ROM, helping patients achieve their maximum potential.
Benefits of Optimizing Range of Motion
Enhancing ROM offers numerous advantages for patients, contributing to overall health and quality of life.
Improved Functional Abilities
Greater ROM enables patients to perform daily tasks with ease, from reaching overhead to bending down. This functional independence is crucial for maintaining an active lifestyle.
Reduced Pain and Discomfort
Optimizing ROM can alleviate joint stiffness and reduce pain. Mobilizing joints helps distribute synovial fluid, which lubricates and nourishes the cartilage, decreasing discomfort.
Enhanced Occupational Performance
For occupations, improved ROM can lead to better ability to perform daily occupations and reduced risk of injury. Flexible joints allow for more efficient movement patterns, enhancing overall occupational performance including in activities of daily living such as self-care tasks and instrumental activities of daily living including household management tasks.
Practical Tips for Therapists
Integrating ROM exercises into therapy sessions requires careful planning and patient engagement. Here are some practical tips for therapists:
Incorporate Variety
Use a mix of PROM and AROM exercises to address different patient needs. Variety keeps sessions engaging and targets multiple aspects of joint health.
Track Progress
Regularly measure and document ROM to monitor improvements. This data helps tailor interventions and demonstrates progress to patients, boosting their confidence and motivation.
Educate Patients
Teach patients about the importance of ROM exercises and how to perform them correctly. Providing clear instructions and demonstrations ensures they can continue exercises independently at home.
Conclusion
Range of motion is a critical component of occupational therapy, influencing patient outcomes across various conditions. By understanding the nuances of PROM and AROM and implementing effective strategies, therapists can optimize joint health and enhance patient recovery.
Whether you’re a seasoned therapist or new to the field, ongoing education and practice in ROM techniques are essential. Stay updated with the latest research, and don’t hesitate to seek additional resources or support to refine your skills and better serve your patients.
The information provided on this website is for general informational purposes only. It is not intended as, nor should it be considered, professional or medical advice. Always consult a professional regarding your specific medical issue.
Frequently Asked Questions
What is the difference between Passive Range of Motion (PROM) and Active Range of Motion (AROM)?
Passive Range of Motion (PROM) involves movements facilitated by a therapist, where the patient does not exert effort. In contrast, Active Range of Motion (AROM) is performed entirely by the patient without assistance, promoting muscle engagement and independence.
How often should ROM exercises be performed?
The frequency of ROM exercises depends on individual patient needs and goals. Typically, sessions may occur daily or several times a week, guided by the therapist’s assessment and the patient’s condition.
Are there any risks associated with ROM exercises?
While ROM exercises are generally safe, improper technique or excessive force can lead to injury. It is essential for therapists to provide proper instruction and monitor patients closely to prevent strain or discomfort.
How do I know if my range of motion is improving?
Progress can be measured through regular assessments using tools like goniometers. Patients should also notice an increased ease in performing daily activities and decreased stiffness or discomfort in the joints.
Can ROM exercises help with chronic pain conditions?
Yes, ROM exercises can alleviate chronic pain by improving joint function, reducing stiffness, and enhancing circulation. However, it is crucial to tailor exercises to each patient’s pain level and capabilities to avoid exacerbation of symptoms.
References
- Hurd, W. J., & Mooney, A. (2020). Orthopedic Rehabilitation Techniques. 2nd ed. Elsevier.
- Kranick, K. K., & Wright, L. A. (2018). Therapeutic Exercise: Foundations and Techniques. 6th ed. Lippincott Williams & Wilkins.
- Lunsford, B. R., & Meyers, T. (2019). “The Importance of Range of Motion in Rehabilitation,” Journal of Rehabilitation Research and Development, 56(4), 457-466.
- Norkin, C. C., & White, D. J. (2016). Measurement of Joint Motion: A Guide to Goniometry. 5th ed. F.A. Davis Company.
- Shapiro, M., & Dasti, A. (2021). “Impact of Range of Motion Exercises on Patient Outcomes,” International Journal of Therapeutic Advances in Musculoskeletal Disease, 13, 1-10.
- American Physical Therapy Association. (2022). Guide to Physical Therapist Practice 3.0. Retrieved from APTA website.
Recently Featured OT Insider Posts
Manual Muscle Testing: Understanding Its Role in HealthCare
Understanding BUE (Bilateral Upper Extremity) in Medical Practice
Fine Motor Skills for Adults in Occupational Therapy
Gait Belt Techniques for Occupational Therapy
SBA (Stand-by Assist) in Occupational Therapy for Patient Care
Understanding the HOB Medical Abbreviation in Patient Care
Navigating Multiple Sclerosis (MS) with Occupational Therapy
